Unveiling the Data Disparities in Women's Health
May 31, 2023
The Data Gender Gap
In the realm of healthcare and life sciences, data reigns supreme. From public health discussions to scientific breakthroughs, data plays a pivotal role. And let's not forget the pandemic, which catapulted the digitalization of healthcare and expanded the availability of health-related data. It's safe to say that data is a game-changer for care delivery, disease prediction, innovation in biopharma and MedTech, and patient outcomes.
But hold on, there's a catch. Despite the exponential growth in healthcare data, there are glaring gaps, especially in women's health. These gaps span the entire data value chain, from defining women's health to diagnosing, tracking, and analyzing data. These disparities have a direct impact on women's health outcomes worldwide, creating blind spots in research, investment decisions, and prioritizing medical advancements. And guess what? Certain subsets of women, such as those from diverse backgrounds, different sexual orientations, and gender identities, are more vulnerable to these gaps and their negative consequences.

Women’s Health is More Than Just the Parts Covered by a Bikini
So, what's the problem? Well, let's start with definitions. Historically, women's health was largely equated with reproductive health (AKA Bikini Medicine). But now, academics and clinicians are embracing a broader perspective. They recognize that sex plays a significant role in the development and progression of many diseases as well as overall biological processes. However, the lack of a universally accepted definition of "women's health" adds to the murkiness.
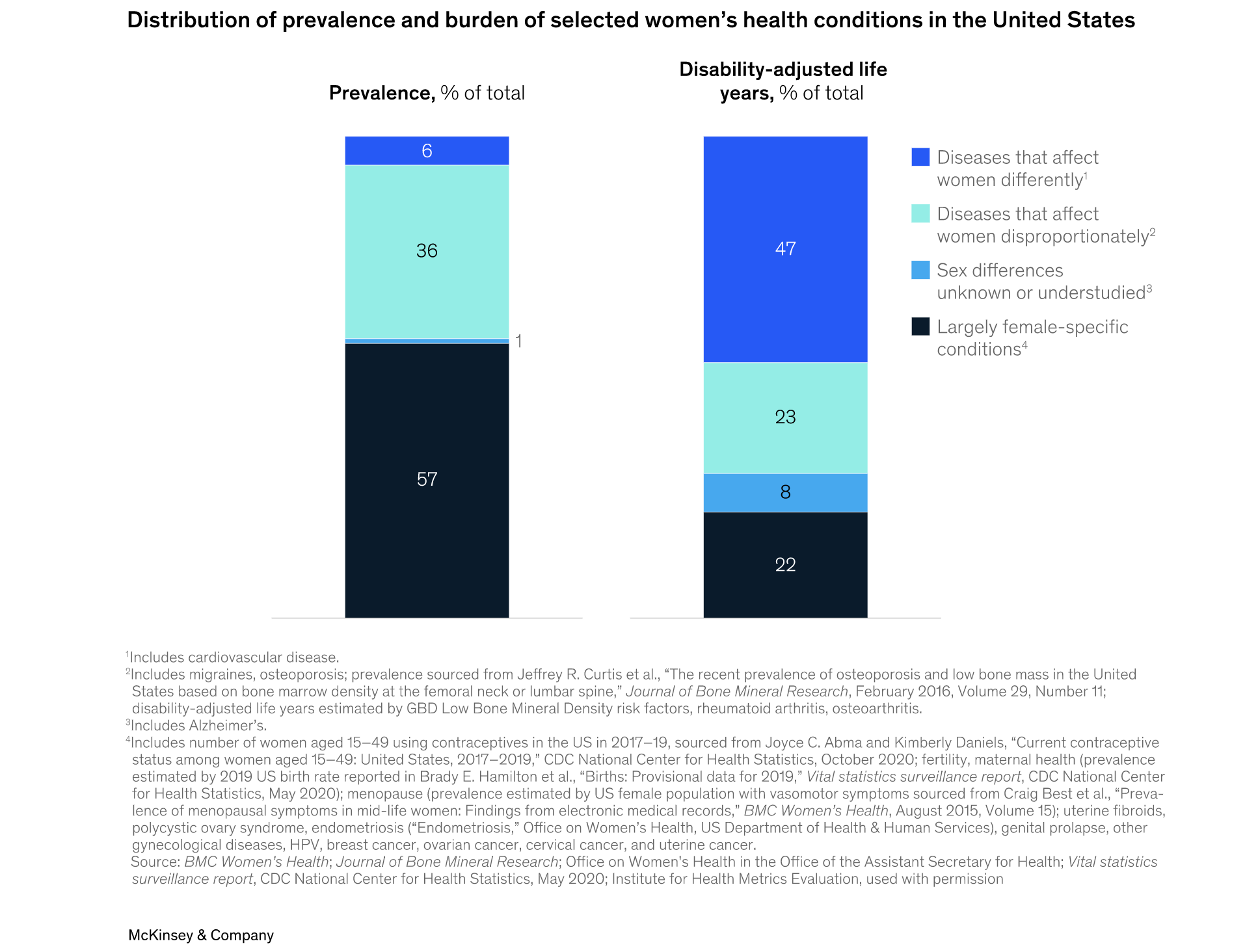
For this article, "women's health" can defined as encompassing both female-specific conditions tied to reproduction or female biology and general health conditions that may affect women differently or disproportionately. Think cardiovascular diseases and autoimmune diseases. Understanding these sex-driven differences is crucial because our current care models often overlook them, leading to varying health outcomes, often to women's disadvantage.

The Invisible Woman
Now, let's talk about data generation. Insurance claims data is a valuable source of insights into health conditions and treatments. But here's the kicker: an analysis of US claims data from January 2019 through August 2022 revealed that the prevalence of women's health conditions is roughly five times higher than the documented diagnoses. In other words, for every diagnosed woman, approximately four go undiagnosed. Meanwhile, the gap between prevalence and diagnoses for men's health conditions narrows significantly. What gives?
This disparity suggests inconsistencies in women's health data across various sources, but it could also reflect structural biases in care delivery. Implicit biases, those unconscious attitudes and beliefs, contribute to diagnostic uncertainty. Sadly, 20% of women report that healthcare providers have ignored or dismissed their symptoms, compared to 14% of men. It's time to address these biases and bridge the gap.
Women Doctors Get It
And guess what else we found? The sex of the diagnosing physician appears to influence the likelihood of diagnosing a condition. In the claims data we analyzed, women were more likely to receive a diagnosis for female-specific conditions like menopause, polycystic ovary syndrome (PCOS), and endometriosis if their physician was a woman. While women represent around 40% of primary care physicians, they accounted for nearly 50% of PCPs documenting diagnoses of these key women's health conditions.
These biases in care delivery are perpetuated during medical training. Shockingly (or at least it should be shocking), many internal-medicine residency programs don't include menopause, contraception, PCOS, or infertility in their core curriculum. And even in programs dedicated to women's health, formal training in menopause medicine is received by fewer than two in ten residents. Let's break this cycle and give women the care they deserve!

Our Male-Dominant Data Disempowers Women
Now, let's shift our focus to data collection. Globally, the quality and quantity of women's health data are far from consistent. Reporting rates for gender-specific healthcare indicators are alarmingly low in many countries, including the US. Even in the areas of Bikini Medicine where representation is higher, less than 10% of countries reported data related to female access to contraception in 2020. This lack of visibility hampers our understanding of women’s health and maternal and child health. We need to shed light on these issues and promote gender equity!
As for data analysis, the traditional metrics used in global epidemiological studies may not capture the true scale of need in women's health. An analysis of the prevalence and burden of disease associated with select women's health conditions using the global burden of disease (GBD) tool found that traditional health metrics fail to accurately reflect the widespread suffering caused by female-specific conditions. Menopause, infertility, endometriosis, and dysmenorrhea—these conditions have a significant impact on women's lives, yet their true burden remains underestimated.
For instance, did you know that menopause interferes with the lives of approximately 80% of women, causing depression in about one-third of them? Or that infertility is linked to higher rates of depression and anxiety, especially in low- and middle-income countries? And let's not forget the excruciating journey of diagnosing endometriosis, with delays and financial burdens that disproportionately affect women. These conditions deserve more attention, understanding, and support. And this is just scratching the surface of what is really needed to understand women’s biology and health overall.
Call For Action
As data enthusiasts, we have the power to change the narrative. It's time to bridge the data gaps, challenge biases, and redefine women's health in a comprehensive and inclusive manner. Together, we can pave the way for a healthier future where no woman is left behind.

